Happy holidays everyone! This post is a holiday special, really only because I’m posting it on Christmas day. Regardless, I hope you enjoy it!
When you think of the types of patients who are treated by a physical therapist, what profile comes to mind? Rather, what condition being treated comes to mind?
Maybe you thought “back pain,” “neck pain,” “ACL tear,” ”rotator cuff,” or “hip or knee replacement.” All of those are 100% accurate, but I wonder…did you think “balance” or “vertigo” or “dizziness”? If you did (and are not a current classmate or physical therapist…or my mother) then hats off to you. If you didn’t, no offense taken. The world of vestibular rehab, for patients and physical therapists alike, is an elusive niche, and for a reason.
I just completed my third rotation out of four, and happened to be working in one of those niche clinics. The first thing I’ll offer is an answer to the question “what is the vestibular system?” The vestibular system, more commonly referred to as the “inner ear,” provides information about the position of your head in space: when the head is still, when it is moving straight like in a car, or up and down like in an elevator, or when you tilt or turn your head. When our vestibular system is in dysfunction, we might experience symptoms such as vertigo, dizziness, motion sensitivity, or a general sense of disequilibrium or “feeling off.” This happens because the information that is getting to our brain under these conditions is inaccurate.
Why does our brain need this information? Well, we’d have a hard time standing upright otherwise. If you’re having trouble appreciating what it is I’m telling you, then try this challenge: Condition 1 – stand in front of a counter or something firm you can grab if this ends poorly; put your feet together so that your base of support on which you stand is now narrow, put your arms by your sides, look ahead, and balance for 20 seconds. Easy? Okay. Condition 2 – try closing your eyes in the same posture. A little harder? Maybe you felt yourself sway a little bit. I have a better one for you still. Condition 3 – find a cushion or a throw pillow to put under your feet, one that doesn’t allow you to feel the floor when you stand on it (if needed, fold up a towel and put underneath the pillow). Again, keep your feet together. You can leave your eyes open for the next 20 seconds. Think you’re a balance master yet? For the final challenge (and please make sure you are still in front of that counter or firm object) …Condition 4 – continue standing on that throw pillow with your feet together, and once you feel like you have your balance, close your eyes, and count to 20 (if you’re a fast counter then maybe set a timer on your phone). How long did you make it? Were you swaying backward or forward, or even side to side? Did you completely lose control? Congratulations, you just had your vestibular world rocked!
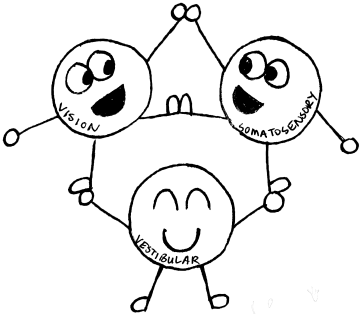
So what happened? Why might you have lost your balance? Why was it so much harder to balance with your eyes closed? In that last scenario, it was not a question of strength. Our ability to balance is the result of what we refer to as sensory integration, meaning that multiple systems are collaborating together to produce balance. Three : our somatosensory system, our visual system, and our vestibular system. In that final challenge, you singled out your vestibular system. There are other motor components to balance that involve control from the cerebellum and other parts of the brain, but that information is not for this post. For now, I’m just focusing on the three systems mentioned above.
The somatosensory system provides afferent information (meaning information that travels toward the brain). It is a tactile (touch) system, allowing your hands to sense an object they are holding, the sole of your foot to sense the ground on which it stands or walks, basically anything to come in contact with your skin in the form of touch and vibration. Are you familiar with the term “diabetic neuropathy”? People who have this condition have an impaired somatosensory component to their balance, and as a result have difficulty sensing the floor beneath their feet. In a sense (pun maybe intended…), they are already walking around essentially a man down from their balance army. When you stood on a cushion or a throw pillow, you nixed your somatosensory system out of the equation, and were then forced to rely on your visual and vestibular system.
Your visual system is your ability to interpret the world around you with sight, depth perception, and has direct neuronal connections to the vestibular system (in other words there are long neurons in the brain that connect the inner ear to the eyes). Without a doubt, we use our visual system as the front man for our ability to balance and remain upright, so much so that it is unconscious. There’s a reason why yoga is less relaxing when we try closing our eyes and holding tree pose…TIMBEEEEEERRRR!
When you stood on the cushion or pillow, you told your somatosensory system to go sit in a corner. Then when you closed your eyes, you voluntarily took out your chess queen of balance, and you called in your vestibular system as your main player. Is yours up to speed?
So why is this important? Why is it crucial that you are able to maintain a certain level of physical balance throughout life? Research studies indicate that inability to maintain condition 4 (from challenge above) less than 20 seconds results in a 3.6-fold increase in odds of falling as an older adult. You use balance every single day, and you are functional because of it. What else is important to know is that physical therapists can help retrain that sensory integration, and recalibrate the way the brain is interpreting signals.
The vestibular system is not just a one-function wonder though. Due to the complex multitude of overlapping and merging pathways in the brain, and blood vessels connections with nerve function, further evidence has revealed a correlation between dizziness/vertigo and loss of balance with: concussions, strokes, whiplash, chronic neck pain, migraines, atherosclerosis, and anxiety to name a few.
Other more every-day occurrences that may offset the how the vestibular system sends information to the brain are ear infections, allergies, sinus infections, and hormone imbalance. Common dietary influences may include too much alcohol, caffeine, or sodium.
BPPV, endolymphatic hydrops or Meniere’s disease, vestibular neuritis, and vestibular migraine are common diagnoses that walk through the doors of a vestibular clinic. Additionally, vestibular rehabilitation specialists often work with audiologists. Hearing tests offer more information besides whether or not you have hearing loss or might need hearing aids. Further, vestibular rehab specialists often refer to and communicate with neurologists and ENTs (ear/nose/throat specialists) to gain additional diagnostic information. It is important to know that though vestibular physical therapists are very capable of treating vestibular dysfunction and improving balance, we can only theorize what is potentially a cause of the problem. The other aforementioned specialists (audiologist, neurologist, ENT) are the ones who can provide are more comprehensive diagnosis. Vestibular rehab is often a very multi-faceted approach, with knowledge needed from multiple minds.
It’s understandable why vestibular rehabilitation is such an elusive specialty. To lose a little professionalism here, it can be a bitch to treat. It’s a combination of providing the right information and instruction, and the patient putting in the time and realizing that results are not instantaneous. Further, remember that medications only suppress symptoms; they can’t fix what the underlying problem is. What it comes down to is that there is a dysfunction in the way the brain is receiving messages, whether the problem is in the brain itself or with the vestibular system. What is awesome though is that the connection between the two can be recalibrated.
I had an awesome experience on my rotation, and this post is not me holding up a large sign reading “I’m going to be a vestibular specialist!” However, it is me saying that a solid training to at least be able to recognize a vestibular component in any patient’s clinical appearance, and know how to give a basic treatment progression is worth the time. There are few true vestibular rehabilitation therapy clinics in number, so that means that someone with a vestibular dysfunction is more likely to walk into a general outpatient setting.
To everyone who has read this and anyone who has found this informative an helpful, I wish you all a Merry Christmas, happy holiday, and a wonderful new year 🙂
-Sarah
Resources:
Agrawal Y et al. The Modified Romberg Balance Test: Normative Data in U.S. Adults. Otology & Neurology. 32:1309-1311. 2011. – Johns Hopkins University School of Medicine
http://geriatrictoolkit.missouri.edu/Agrawal-Romberg-EC-compliant-norms-2011.pdf
Wei W, et al. Presence of anxiety and depression symptoms affects the first time treatment efficacy and recurrence of BPPV. Front Neurol. 9(178); March 2018
Walker A, Kantaris X, Chambers M. Understanding therapeutic approaches to anxiety in vestibular rehabilitations: a qualitative study of specialist physiotherapists in the UK. Disability and Rehabilitation. 40(7):829-835. 2018
Balaban C. Projections from parabrachial nucleus to the vestibular nuclei: potential substrates for autonomic and limbic influences on vestibular responses. Brain Research. 996(1);126-137. January 2004
Bittar R, Santos M, Mezalira R. Glucose metabolism disorders and vestibular manifestations: evaluation through computerized dynamic posturography. Brazilian Journal of Otorhinolaryngology. 82(4):372-376. May 2016.
